Congenital and Acquired Angioedema
Содержимое
Learn about the causes, symptoms, and treatment options for congenital and acquired angioedema, a condition characterized by sudden and recurring swelling in the deep layers of the skin and mucous membranes. Understand the differences between these two types of angioedema and how they can affect your daily life.
Angioedema is a condition characterized by swelling in the deeper layers of the skin and mucous membranes. It can occur as a result of various factors, including an allergic reaction, an inherited disorder, or an underlying medical condition. In this article, we will focus on two types of angioedema: congenital and acquired.
Congenital angioedema is a rare genetic disorder that is usually inherited. It is caused by a deficiency or dysfunction of a protein called C1 inhibitor. This protein plays a crucial role in regulating the immune system and preventing the release of certain substances that can cause swelling. People with congenital angioedema may experience recurrent episodes of swelling that can affect different parts of the body, including the face, limbs, and internal organs.
Acquired angioedema, on the other hand, is not inherited and can occur later in life. It is typically associated with certain medical conditions, such as autoimmune disorders, lymphoproliferative disorders, or certain types of cancer. Acquired angioedema can also be caused by the use of certain medications or exposure to certain triggers, such as infections or emotional stress.
The symptoms of angioedema may vary depending on the type and severity of the condition. Common symptoms include swelling, redness, and pain in the affected area. In some cases, angioedema may also be accompanied by other symptoms, such as difficulty breathing, abdominal pain, or vomiting. It is important to seek medical attention if you experience any symptoms of angioedema, as the condition can be potentially life-threatening in severe cases.
Treatment for angioedema may involve medications to relieve symptoms and prevent future episodes. Antihistamines and corticosteroids may be prescribed to reduce inflammation and swelling. In some cases, medications that inhibit the production of certain substances involved in the immune response may be used. Additionally, patients may be advised to avoid triggers that can cause or worsen angioedema, such as certain foods, medications, or environmental factors.
In conclusion, angioedema is a condition characterized by swelling in the deeper layers of the skin and mucous membranes. It can be caused by various factors, including an allergic reaction, an inherited disorder, or an underlying medical condition. Congenital and acquired angioedema are two types of the condition that differ in their causes and presentation. If you experience any symptoms of angioedema, it is important to seek medical attention for proper diagnosis and treatment.
Congenital Angioedema
Congenital angioedema is a rare genetic disorder that is characterized by recurring episodes of angioedema. It is inherited in an autosomal dominant pattern, meaning that individuals with a family history of angioedema have a 50% chance of passing the condition onto their children.
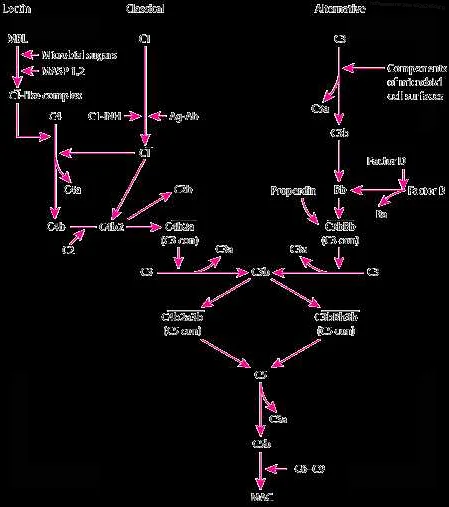
This condition is caused by a deficiency or dysfunction of the C1 inhibitor protein, which plays an important role in regulating the complement and kinin pathways. Without functional C1 inhibitor, there is an overproduction of bradykinin, a vasoactive peptide that leads to increased vascular permeability and the characteristic swelling seen in angioedema.
The symptoms of congenital angioedema can vary in severity and may include swelling of the face, lips, tongue, throat, and extremities. Swelling of the gastrointestinal tract can also occur, leading to abdominal pain, nausea, and vomiting. These episodes can last anywhere from a few hours to several days, and can be life-threatening if the airway becomes compromised.
Diagnosis of congenital angioedema is typically based on clinical presentation, family history, and laboratory testing. Laboratory tests may include measuring C1 inhibitor levels and function, as well as complement levels. Genetic testing may also be done to identify mutations in the C1 inhibitor gene.
Treatment for congenital angioedema focuses on preventing and managing attacks. This can include the use of medications such as C1 inhibitor replacement therapy, bradykinin receptor antagonists, antifibrinolytic agents, and corticosteroids. Prophylactic treatment may also be used to reduce the frequency and severity of attacks.
In addition to medical management, individuals with congenital angioedema should also be educated on identifying triggers and implementing strategies to avoid them. Triggers may include certain medications, infections, trauma, and emotional stress. It is also important for individuals with congenital angioedema to have an emergency action plan in place in case of a severe attack.
| Swelling of the face, lips, tongue, throat, and extremities | C1 inhibitor replacement therapy |
| Abdominal pain, nausea, and vomiting | Bradykinin receptor antagonists |
| Difficulty breathing | Antifibrinolytic agents |
| Emergency action plan | Corticosteroids |
Causes of Congenital Angioedema
Congenital angioedema is a hereditary condition that is caused by genetic mutations. There are three types of congenital angioedema, each with different underlying genetic causes:
- Type I: This type is caused by a deficiency or dysfunction of a protein called C1 esterase inhibitor (C1-INH). The gene responsible for producing C1-INH is called SERPING1. Mutations in this gene can lead to decreased or ineffective production of C1-INH, resulting in the development of angioedema.
- Type II: Type II congenital angioedema is also caused by mutations in the SERPING1 gene. However, in this type, the mutations result in the production of abnormal forms of C1-INH that do not function properly.
- Type III: Type III congenital angioedema is less common and is primarily seen in women. It is caused by mutations in a different gene called F12. These mutations lead to increased activation of a protein called factor XII, which in turn leads to excessive production of bradykinin, a substance that causes blood vessels to dilate and leak fluid, resulting in angioedema.
It is important to note that congenital angioedema is a genetic condition and is not related to allergies or histamine release, which are the underlying causes of acquired angioedema.
Understanding the genetic causes of congenital angioedema is crucial for accurate diagnosis and targeted treatment strategies. Genetic testing can help identify the specific gene mutations responsible for the condition, which can inform treatment decisions and help improve patient outcomes.
Symptoms of Congenital Angioedema
Congenital angioedema is a rare genetic disorder that primarily affects the immune system and can lead to recurrent episodes of swelling in various parts of the body. These episodes can last for a few hours to several days and can be life-threatening if they affect the airways.
The symptoms of congenital angioedema can vary from person to person, but the most common signs include:
- Sudden and severe swelling of the face, lips, tongue, or throat
- Swelling in the hands, feet, or genitals
- Abdominal pain and cramping
- Nausea and vomiting
- Difficulty breathing
- Hoarseness or difficulty speaking
- Difficulty swallowing
- Itchy or red skin
These symptoms can occur spontaneously or be triggered by factors such as stress, trauma, infections, hormonal changes, or certain medications. It is important to note that not all individuals with congenital angioedema experience the same symptoms or have the same frequency of attacks.
If you or someone you know is experiencing any of these symptoms, it is important to seek medical attention immediately. Prompt diagnosis and treatment can help manage the symptoms and prevent potentially life-threatening complications.
Treatment for Congenital Angioedema
Congenital angioedema is a rare genetic condition that requires long-term management and treatment. The primary goal of treatment is to prevent and manage acute attacks, as well as to improve the patient’s overall quality of life.
1. Medications:
Medications are the key component of managing congenital angioedema. The most common medications used are:
- Plasma-derived C1 inhibitor concentrate: This is the most effective treatment for acute attacks and can be administered intravenously. It works by replenishing the deficient or dysfunctional C1 inhibitor in the body.
- Recombinant human C1 inhibitor: This is another option for acute attack treatment and works in a similar way to plasma-derived C1 inhibitor concentrate.
- Androgens: Androgens, such as danazol, can help prevent attacks by increasing the production of C1 inhibitor. However, they have significant side effects and are usually reserved for patients who do not respond to other treatments.
2. Trigger avoidance:
Identifying and avoiding triggers can help reduce the frequency and severity of angioedema attacks. Common triggers include certain foods, medications, insect bites, and emotional stress. Keeping a diary of symptoms and triggers can be helpful in identifying patterns.
3. Supportive measures:
During an acute attack, supportive measures can help alleviate symptoms and promote comfort. These measures may include:
- Rest and relaxation: Taking time to rest and relax can help reduce stress and ease symptoms.
- Cold compresses: Applying cold compresses to affected areas can help reduce swelling and provide temporary relief.
- Elevation: Elevating the affected area can help reduce swelling and promote drainage.
4. Regular follow-up:
Patients with congenital angioedema should have regular follow-up appointments with their healthcare provider to monitor their condition, adjust treatment as needed, and assess overall health and well-being.
It is important for individuals with congenital angioedema to work closely with their healthcare team to develop an individualized treatment plan that meets their specific needs and helps manage their condition effectively.