Functional Peripheral Arterial Disease: An Overview
Содержимое
Get a comprehensive overview of functional peripheral arterial disease, including its causes, symptoms, diagnosis, and treatment options. Understand how this condition affects blood flow to the limbs and the importance of early detection and management. Explore the latest advancements in medical interventions and lifestyle modifications for functional peripheral arterial disease.
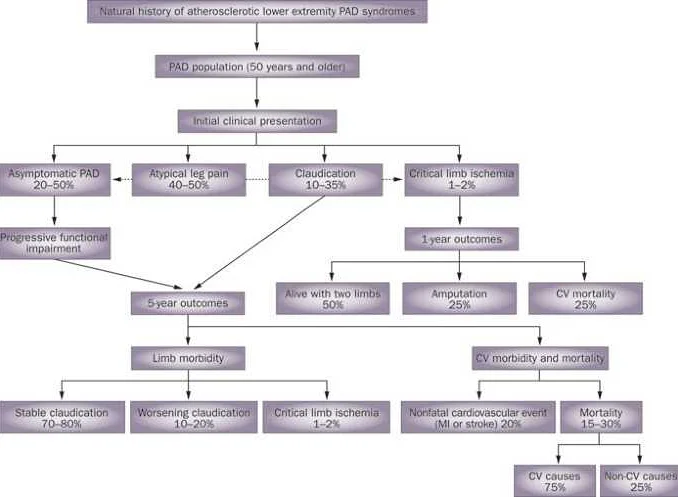
Peripheral Arterial Disease (PAD) refers to the narrowing or blockage of arteries in the peripheral regions of the body, most commonly in the lower limbs. While atherosclerosis is the leading cause of PAD, there is another form of the disease known as functional PAD, which is characterized by arterial dysfunction without significant structural changes.
In functional PAD, the arteries do not exhibit the typical signs of atherosclerosis, such as plaque formation or calcification. Instead, the dysfunction is attributed to abnormalities in the endothelium, the inner lining of the blood vessels. Endothelial dysfunction can lead to impaired vasodilation, increased vascular tone, and reduced blood flow to the affected areas.
This comprehensive overview aims to provide a detailed understanding of functional PAD, its pathophysiology, clinical presentation, diagnostic methods, and available treatment options. By exploring the intricacies of this lesser-known form of PAD, healthcare professionals can better recognize and manage patients with functional PAD, ultimately improving their quality of life.
Causes and Risk Factors
Functional peripheral arterial disease (PAD) can have various causes and risk factors. Some of the common causes and risk factors include:
| Smoking | Smoking is one of the leading causes of PAD. The toxins present in cigarettes can damage the blood vessels, leading to reduced blood flow and oxygen supply to the limbs. Smokers are at a significantly higher risk of developing PAD compared to non-smokers. |
| Diabetes | Diabetes is another major risk factor for PAD. High blood sugar levels can cause damage to the blood vessels and increase the risk of developing atherosclerosis. People with diabetes are more likely to develop PAD at a younger age and have a higher risk of complications. |
| High Blood Pressure | Uncontrolled high blood pressure can damage the arteries and increase the risk of developing PAD. The constant pressure on the arterial walls can cause them to become thick and narrow, restricting the blood flow to the limbs. |
| High Cholesterol | Elevated levels of cholesterol in the blood can contribute to the development of atherosclerosis, a condition characterized by the buildup of plaques in the arteries. These plaques can narrow the arteries and reduce blood flow, leading to PAD. |
| Family History | Having a family history of PAD can increase the risk of developing the condition. Genetics can play a role in the development of PAD, and individuals with a family history should be more vigilant about their cardiovascular health. |
| Age | Advancing age is a common risk factor for PAD. As people get older, the blood vessels tend to become less elastic and more prone to damage. The risk of developing PAD increases significantly after the age of 50. |
| Gender | Men are more likely to develop PAD compared to women. However, women with diabetes have an equal risk of developing the condition. Hormonal factors and lifestyle choices may contribute to the gender disparity. |
It is important to understand the causes and risk factors associated with functional PAD in order to prevent its development or manage the condition effectively. Lifestyle modifications, such as quitting smoking, maintaining a healthy weight, exercising regularly, and managing underlying health conditions, can help reduce the risk of developing PAD.
Symptoms and Diagnosis
Peripheral arterial disease (PAD) often presents with a variety of symptoms that can vary depending on the severity of the disease. Some common symptoms include:
- Intermittent claudication: This refers to pain or cramping in the leg muscles that occurs during physical activity and usually subsides with rest.
- Numbness or weakness: Patients with PAD may experience a tingling sensation, numbness, or weakness in their legs or feet.
- Coolness or discoloration: The affected leg or foot may feel cool to the touch or have a bluish or pale appearance.
- Skin changes: PAD can cause the skin on the legs or feet to become shiny, thin, or develop ulcers.
- Slow-healing wounds: Due to reduced blood flow, wounds on the legs or feet may take longer to heal.
If you are experiencing any of these symptoms, it is important to see a healthcare professional for a proper diagnosis. The diagnosis of PAD typically involves a combination of medical history, physical examination, and diagnostic tests. The healthcare provider may perform a physical examination to evaluate the pulses in the legs and feet, as well as assess any changes in the skin or wounds. They may also use non-invasive tests such as ankle-brachial index (ABI) measurement, which compares blood pressure in the ankle to blood pressure in the arm, or doppler ultrasound to assess blood flow in the arteries.
In some cases, additional imaging tests such as computed tomography angiography (CTA) or magnetic resonance angiography (MRA) may be ordered to obtain detailed images of the blood vessels and identify any blockages or narrowing. These tests can help determine the severity and location of the arterial disease.
Early diagnosis of PAD is crucial in order to prevent progression of the disease and reduce the risk of complications. If you experience any symptoms related to PAD, it is important to seek medical attention promptly for appropriate evaluation and treatment.
Treatment Options
Functional peripheral arterial disease (PAD) requires a comprehensive approach to management. The treatment options for functional PAD depend on several factors, including the severity of the disease, the patient’s overall health, and their individual preferences.
1. Lifestyle modifications: Lifestyle changes play a crucial role in managing functional PAD. These may include quitting smoking, engaging in regular exercise, maintaining a healthy weight, and following a heart-healthy diet. Lifestyle modifications can help improve symptoms and slow disease progression.
2. Medications: Medications may be prescribed to manage symptoms and reduce the risk of complications. Commonly used medications include antiplatelet agents, such as aspirin or clopidogrel, to prevent blood clots, and statins to reduce cholesterol levels.
3. Interventional procedures: In some cases, interventional procedures may be recommended to alleviate symptoms and improve blood flow. These may include angioplasty, in which a balloon is used to open narrowed blood vessels, or stenting, in which a small mesh tube is inserted to keep the blood vessel open.
4. Surgery: In severe cases of functional PAD, surgery may be necessary. Procedures such as bypass grafting can be performed to reroute blood flow around blocked or narrowed arteries. Surgical intervention is typically considered when other treatment options have failed.
5. Rehabilitation: Rehabilitation programs can help patients with functional PAD improve their overall cardiovascular health. These programs may include supervised exercise sessions, education on managing risk factors, and emotional support.
6. Adjunctive therapies: Some complementary and alternative therapies may be used as adjunctive treatments for functional PAD. These may include acupuncture, massage, or herbal supplements. However, it is important to consult with a healthcare professional before trying any alternative therapies.
Functional PAD is a chronic condition that requires ongoing management. A multidisciplinary approach involving healthcare professionals from various specialties is often necessary to provide comprehensive care for patients with functional PAD.
Prevention and Lifestyle Changes
Preventing functional peripheral arterial disease (PAD) involves making significant lifestyle changes. It is important to adopt a healthy lifestyle to reduce the risk of developing PAD or to slow the progression of the disease. The following lifestyle changes are recommended:
- Quit smoking: Smoking is a major risk factor for PAD and can greatly increase the likelihood of developing the disease. Quitting smoking is crucial for preventing and managing PAD.
- Exercise regularly: Engaging in regular physical activity can improve circulation and help prevent PAD. Aim for at least 30 minutes of moderate exercise, such as brisk walking or cycling, most days of the week.
- Maintain a healthy weight: Obesity is another risk factor for PAD. By maintaining a healthy weight, you can reduce the strain on your arteries and lower your risk of developing the disease.
- Eat a nutritious diet: A healthy diet low in saturated and trans fats, cholesterol, and sodium can help prevent PAD. Focus on consuming fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Manage blood pressure and cholesterol levels: High blood pressure and high cholesterol are significant risk factors for PAD. It is important to regularly check your blood pressure and cholesterol levels and take steps to manage them within a healthy range.
- Control diabetes: Diabetes increases the risk of developing PAD. If you have diabetes, it is crucial to manage your blood sugar levels through proper diet, exercise, and medication as prescribed by your healthcare provider.
- Limit alcohol consumption: Excessive alcohol consumption can contribute to the development of PAD. It is recommended to limit alcohol intake to moderate levels (up to one drink per day for women and up to two drinks per day for men).
- Manage stress: Chronic stress can have a negative impact on your overall health, including your circulatory system. Find healthy ways to manage stress, such as practicing relaxation techniques, engaging in hobbies, or seeking support from loved ones.
By implementing these lifestyle changes, you can reduce your risk of developing functional PAD and improve your overall cardiovascular health. It is important to consult with your healthcare provider for personalized recommendations and guidance.