Hypertensive Arteriolar Nephrosclerosis
Содержимое
Hypertensive arteriolar nephrosclerosis is a condition in which the small blood vessels in the kidneys become damaged due to high blood pressure. This can lead to kidney dysfunction and may require medical intervention. Learn more about the causes, symptoms, and treatment options for hypertensive arteriolar nephrosclerosis.
Hypertensive arteriolar nephrosclerosis, also known as hypertensive nephrosclerosis or hypertensive kidney disease, is a progressive kidney condition that is caused by high blood pressure. It is a common and serious complication of hypertension, affecting millions of people worldwide.
This condition develops over time as chronic high blood pressure damages the small blood vessels in the kidneys, known as arterioles. As a result, the kidneys are unable to filter waste products and excess fluid from the blood effectively. Over time, this can lead to kidney dysfunction and the development of various signs and symptoms.
Common symptoms of hypertensive arteriolar nephrosclerosis include persistent high blood pressure, proteinuria (presence of excess protein in the urine), edema (swelling), and gradual loss of kidney function. In some cases, the condition may progress to end-stage renal disease, requiring dialysis or a kidney transplant for survival.
While the exact cause of hypertensive arteriolar nephrosclerosis is not fully understood, it is primarily associated with uncontrolled high blood pressure. Other risk factors that can contribute to the development of this condition include diabetes, obesity, smoking, and a family history of kidney disease.
Treatment for hypertensive arteriolar nephrosclerosis focuses on managing and controlling blood pressure. Medications such as angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are commonly prescribed to help lower blood pressure and protect the kidneys from further damage. Lifestyle modifications, such as adopting a healthy diet, exercising regularly, and quitting smoking, are also important in managing this condition.
In conclusion, hypertensive arteriolar nephrosclerosis is a serious kidney condition that is caused by chronic high blood pressure. It can lead to kidney dysfunction and the development of various symptoms. Early diagnosis and treatment are crucial in managing this condition and preventing further complications.
What Is Hypertensive Arteriolar Nephrosclerosis?
Hypertensive arteriolar nephrosclerosis, also known as hypertensive renal disease, is a condition that affects the kidneys and is caused by long-standing high blood pressure. It is a common form of kidney disease and a leading cause of end-stage renal disease (ESRD), a condition in which the kidneys fail to function properly.
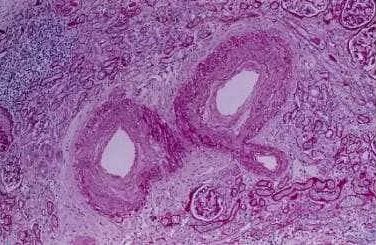
In this condition, the small blood vessels in the kidneys, known as arterioles, become damaged due to the elevated pressure of the blood flow. This damage restricts blood flow to the kidneys, which leads to the formation of scar tissue and the impairment of kidney function over time.
Hypertensive arteriolar nephrosclerosis often develops gradually and may not cause noticeable symptoms in the early stages. However, as the condition progresses, symptoms such as swelling in the legs and ankles, decreased urine output, fatigue, and high blood pressure may occur.
Treating hypertensive arteriolar nephrosclerosis involves managing and controlling blood pressure levels. Medications such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) are commonly prescribed to help lower blood pressure and reduce the strain on the kidneys. Lifestyle changes such as following a low-sodium diet, exercising regularly, and limiting alcohol consumption can also help manage the condition.
In severe cases, where kidney function is significantly impaired, dialysis or kidney transplantation may be necessary to maintain overall health and manage the symptoms of end-stage renal disease.
Overall, early detection and management of high blood pressure are crucial in preventing or slowing the progression of hypertensive arteriolar nephrosclerosis and its associated complications. Regular blood pressure monitoring and routine check-ups with a healthcare provider can help identify and address any potential issues before they worsen.
Causes of Hypertensive Arteriolar Nephrosclerosis
Hypertensive arteriolar nephrosclerosis, also known as hypertensive nephropathy, is a condition characterized by the narrowing and hardening of the small blood vessels in the kidneys, resulting from long-standing high blood pressure. This condition can lead to kidney damage and ultimately, chronic kidney disease.
The primary cause of hypertensive arteriolar nephrosclerosis is uncontrolled high blood pressure. When blood pressure remains consistently elevated, it puts excessive pressure on the delicate blood vessels in the kidneys, causing them to become narrower and thicker over time. This increased resistance to blood flow impairs the kidneys’ ability to filter waste products and excess fluid from the bloodstream effectively.
Other factors that may contribute to the development of hypertensive arteriolar nephrosclerosis include:
- Diabetes: Individuals with both high blood pressure and diabetes are at an increased risk of developing this condition.
- Advanced age: Hypertensive arteriolar nephrosclerosis is more common in older adults.
- Genetics: Some individuals may have a genetic predisposition to developing kidney damage in response to high blood pressure.
- Obesity: Excess body weight can contribute to high blood pressure and increase the risk of kidney damage.
- Smoking: Tobacco use can raise blood pressure and impair kidney function.
It is essential to manage and control high blood pressure to prevent the development or progression of hypertensive arteriolar nephrosclerosis. Lifestyle modifications, such as maintaining a healthy weight, following a balanced diet, exercising regularly, quitting smoking, and limiting alcohol intake, can help to control blood pressure and reduce the risk of kidney damage.
In some cases, medications may be necessary to lower blood pressure and protect the kidneys. These may include angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), diuretics, and calcium channel blockers. Regular monitoring of blood pressure and kidney function is also crucial for individuals with hypertensive arteriolar nephrosclerosis.
Symptoms of Hypertensive Arteriolar Nephrosclerosis
The symptoms of hypertensive arteriolar nephrosclerosis may vary depending on the stage of the disease. In the early stages, patients may not experience any symptoms, making it difficult to detect the condition. However, as the disease progresses, the following symptoms may occur:
– High blood pressure: Hypertensive arteriolar nephrosclerosis is often associated with uncontrolled high blood pressure. Persistent high blood pressure can damage the blood vessels in the kidneys, leading to the development of nephrosclerosis.
– Decreased urine output: As the disease progresses, the kidneys may lose their ability to filter blood effectively, resulting in a decrease in urine production. This can lead to a buildup of waste products and fluid retention in the body.
– Swelling: Fluid retention caused by impaired kidney function can manifest as swelling in the feet, ankles, and legs. This swelling, known as edema, can also occur in the face and hands.
– Fatigue: kidney damage can lead to anemia, a condition characterized by a decrease in red blood cells. Anemia can cause fatigue, weakness, and shortness of breath.
– Changes in urine: The presence of blood in the urine (hematuria) or foamy urine (proteinuria) may indicate kidney damage caused by nephrosclerosis. These changes in urine color or consistency should not be ignored and require medical attention.
– Increased frequency of urination: As the kidneys lose their ability to concentrate urine, patients may experience increased frequency of urination, particularly at night (nocturia).
If you are experiencing any of these symptoms, it is important to seek medical attention for a proper diagnosis and treatment. Prompt management of hypertensive arteriolar nephrosclerosis can help prevent further kidney damage and complications.
Diagnosis and Risk Factors
Hypertensive arteriolar nephrosclerosis is typically diagnosed through a combination of clinical evaluation, medical history, and diagnostic tests. The diagnosis is often made when a patient with a history of hypertension presents with symptoms such as proteinuria, hematuria, or a decline in kidney function.
Medical professionals will also consider the patient’s risk factors when making a diagnosis. Some of the risk factors for hypertensive arteriolar nephrosclerosis include:
- Hypertension: Uncontrolled high blood pressure is the primary risk factor for hypertensive arteriolar nephrosclerosis. Individuals with long-standing, uncontrolled hypertension are at a higher risk of developing kidney damage.
- Age: The risk of developing hypertensive arteriolar nephrosclerosis increases with age. Older individuals are more likely to have long-standing, uncontrolled hypertension, which can lead to kidney damage over time.
- Obesity: Being overweight or obese can contribute to the development of hypertension, which increases the risk of hypertensive arteriolar nephrosclerosis.
- Diabetes: Individuals with diabetes are more prone to developing hypertension and are at an increased risk of developing hypertensive arteriolar nephrosclerosis.
- Smoking: Smoking damages blood vessels and can lead to hypertension, increasing the risk of hypertensive arteriolar nephrosclerosis.
- Family history: Having a family history of hypertension or kidney disease increases the risk of developing hypertensive arteriolar nephrosclerosis.
If hypertensive arteriolar nephrosclerosis is suspected, further diagnostic tests may be performed to confirm the diagnosis and assess the extent of kidney damage. These tests can include blood tests, urine tests, imaging studies such as ultrasound or CT scan, and a kidney biopsy if necessary.
It is important for individuals with risk factors to manage their blood pressure and overall health to reduce the risk of developing hypertensive arteriolar nephrosclerosis. This can be achieved through a combination of lifestyle changes, such as maintaining a healthy weight, exercising regularly, eating a balanced diet, quitting smoking, and managing any underlying medical conditions like diabetes.
Regular check-ups with a healthcare provider are also important for monitoring blood pressure and kidney function, especially for individuals with risk factors for hypertensive arteriolar nephrosclerosis.