Mitral Regurgitation and Its Treatment
Содержимое
Learn about mitral regurgitation, a heart valve disorder characterized by the leakage of blood from the left ventricle back into the left atrium. Discover the various treatment options available, including medication, lifestyle changes, and surgical interventions.
Mitral regurgitation is a heart condition characterized by the leakage of blood from the left ventricle into the left atrium through the mitral valve, instead of flowing forward into the aorta. This backflow of blood can lead to various symptoms and complications, making early diagnosis and management crucial.
Common symptoms of mitral regurgitation include shortness of breath, fatigue, and heart palpitations. As the condition progresses, individuals may also experience cough, chest pain, and swelling in the legs and feet. These symptoms can significantly impact a person’s quality of life and should not be ignored.
There are several causes of mitral regurgitation, including age-related degeneration of the valve, rheumatic heart disease, congenital heart defects, and certain infections. Additionally, heart attacks and other cardiac conditions can also lead to damage to the mitral valve, resulting in regurgitation.
Diagnosing mitral regurgitation typically involves a thorough physical examination, listening to the heart sounds, and performing diagnostic tests such as echocardiography, electrocardiogram, and chest x-ray. These tests help determine the severity of the condition and identify any underlying causes or complications.
Treatment options for mitral regurgitation depend on the severity and underlying cause of the condition. In mild cases, medication may be prescribed to manage symptoms and prevent further damage to the heart. However, in more severe cases, surgical intervention may be necessary to repair or replace the mitral valve.
Overall, understanding the symptoms, causes, diagnosis, and treatment options of mitral regurgitation is essential for both individuals living with the condition and healthcare professionals involved in their care. Early detection and appropriate management can significantly improve outcomes and quality of life for patients with mitral regurgitation.
Symptoms of Mitral regurgitation
Mitral regurgitation is a heart condition that occurs when the mitral valve in the heart does not close properly, leading to blood leaking backward into the left atrium. This can cause a range of symptoms, which can vary in severity depending on the extent of the regurgitation.
Common symptoms of mitral regurgitation include:
| 1. Shortness of breath: | This is a common symptom of mitral regurgitation, as the leaking of blood into the left atrium can lead to a buildup of fluid in the lungs. |
| 2. Fatigue: | Feeling tired or weak without any obvious reason can be a symptom of mitral regurgitation. The heart has to work harder to compensate for the leaky valve, which can lead to fatigue. |
| 3. Heart palpitations: | Irregular or rapid heartbeats can occur as a result of the mitral valve not closing properly. This can cause a fluttering or pounding sensation in the chest. |
| 4. Swelling of the ankles and feet: | As blood flow is affected by the regurgitation, fluid can accumulate in the lower extremities, leading to swelling in the ankles and feet. |
| 5. Coughing: | The buildup of fluid in the lungs can also cause a persistent cough, sometimes accompanied by pink-tinged phlegm. |
| 6. Chest pain: | While not as common, some people with mitral regurgitation may experience chest pain or discomfort, especially during physical activity. |
If you are experiencing any of these symptoms, it is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment options.
Causes of Mitral regurgitation
Mitral regurgitation occurs when the mitral valve, located between the left atrium and left ventricle of the heart, does not close properly. This allows blood to flow backward from the left ventricle into the left atrium instead of moving forward into the aorta and the rest of the body. There are several possible causes of mitral regurgitation:
| 1. Mitral valve prolapse: | This is the most common cause of mitral regurgitation. It occurs when the mitral valve flaps do not close properly and bulge into the left atrium during ventricular contraction. Mitral valve prolapse can be congenital or develop later in life. |
| 2. Mitral valve stenosis: | This is a condition where the mitral valve becomes narrowed, restricting blood flow from the left atrium to the left ventricle. The increased pressure in the left atrium can lead to mitral regurgitation. |
| 3. Rheumatic heart disease: | Rheumatic fever, caused by an untreated streptococcal infection, can damage the mitral valve and lead to mitral regurgitation. This condition is less common in developed countries due to the availability of antibiotics. |
| 4. Infective endocarditis: | This is an infection of the inner lining of the heart chambers and valves. If the mitral valve is affected, it can lead to mitral regurgitation. |
| 5. Congenital heart defects: | Some people are born with abnormalities in the structure of the mitral valve, which can cause mitral regurgitation. |
| 6. Heart attack: | A heart attack can damage the muscles and tissues surrounding the mitral valve, affecting its function and causing mitral regurgitation. |
| 7. Other causes: | Other less common causes of mitral regurgitation include connective tissue disorders, certain medications, and radiation therapy to the chest. |
If you experience symptoms of mitral regurgitation or have risk factors for developing the condition, it is important to seek medical attention for diagnosis and treatment options.
Diagnosis of Mitral regurgitation
Diagnosing mitral regurgitation involves a thorough evaluation of the patient’s medical history, physical examination, and diagnostic tests.
During the physical examination, a healthcare provider will listen to the patient’s heart using a stethoscope. The presence of a heart murmur, specifically a systolic murmur, may indicate mitral regurgitation. The intensity, timing, and location of the murmur can provide additional clues about the severity and nature of the condition.
Diagnostic tests commonly used to confirm the diagnosis of mitral regurgitation include:
- Echocardiography: This ultrasound test allows healthcare providers to visualize the structure and function of the heart, including the mitral valve. It can help determine the severity of mitral regurgitation, assess the size of the left atrium and ventricle, and evaluate the overall condition of the heart.
- Electrocardiogram (ECG): This non-invasive test records the electrical activity of the heart. It can help detect any abnormal heart rhythms or signs of heart muscle damage.
- Chest X-ray: This imaging test can reveal any changes in the size or shape of the heart and lungs. It can also help identify any underlying conditions that may be causing or contributing to mitral regurgitation.
- Cardiac catheterization: This invasive test involves inserting a thin tube (catheter) into a blood vessel and guiding it to the heart. It allows for direct measurement of pressures within the heart chambers and can help identify the cause and severity of mitral regurgitation.
In some cases, additional tests may be necessary to further evaluate the patient’s condition or to determine the most appropriate treatment approach. These may include stress tests, cardiac MRI, or other specialized imaging studies.
It is important to accurately diagnose mitral regurgitation to guide appropriate treatment decisions and to monitor the progression of the condition over time. Regular follow-up appointments and ongoing evaluation are typically recommended for individuals with mitral regurgitation.
Treatment options for Mitral regurgitation
Treatment for mitral regurgitation depends on the severity of the condition and the symptoms experienced by the patient. In some cases, no treatment may be necessary if the regurgitation is mild and not causing any symptoms. The doctor will closely monitor the condition and recommend regular check-ups to ensure that the regurgitation does not worsen over time.
If the mitral regurgitation is moderate to severe, or if it is causing symptoms such as shortness of breath, fatigue, or chest pain, treatment may be required. The treatment options for mitral regurgitation include:
1. Medications: In some cases, medications may be prescribed to manage the symptoms of mitral regurgitation. These medications can help to reduce the workload on the heart and ease the symptoms. Commonly prescribed medications include diuretics to reduce fluid build-up, beta blockers to slow the heart rate, and ACE inhibitors to lower blood pressure.
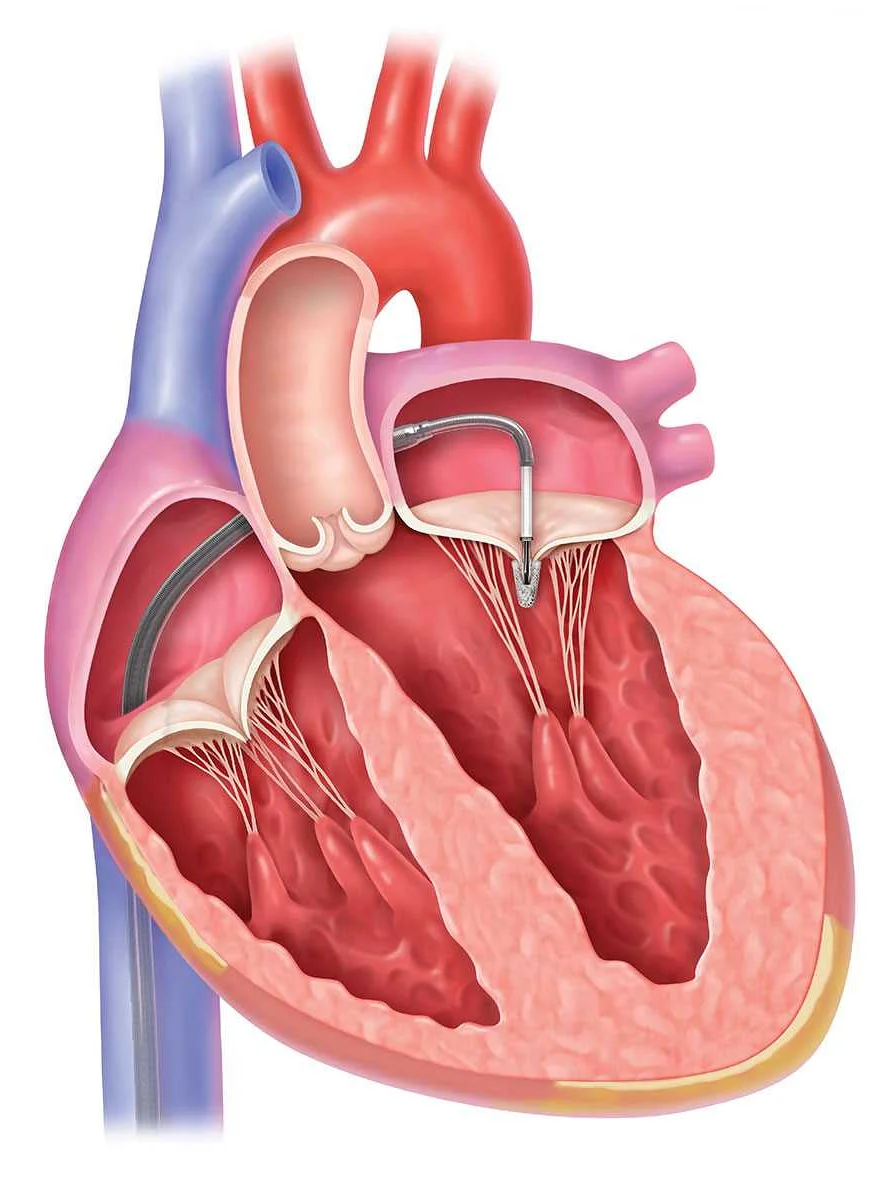
2. Surgery: In more severe cases of mitral regurgitation, surgery may be necessary to repair or replace the mitral valve. Valve repair is typically the preferred option, as it allows the patient to retain their own valve. Valve replacement may be necessary if the damage is too extensive. Surgical procedures may involve minimally invasive techniques or open-heart surgery, depending on the individual case.
3. Transcatheter Mitral Valve Repair (TMVR): TMVR is a minimally invasive procedure that uses a catheter to repair the mitral valve. It is an option for patients who are not suitable candidates for surgery. The catheter is threaded through a blood vessel to the heart, where a device is used to repair the valve. TMVR offers a less invasive alternative to open-heart surgery and can be effective in improving symptoms and reducing mitral regurgitation.
4. Watchful waiting: In some cases, if the patient is not experiencing severe symptoms and the regurgitation is not worsening, the doctor may recommend a watchful waiting approach. This involves regular check-ups to monitor the condition and symptoms, with the option to pursue treatment if necessary.
It is important for individuals with mitral regurgitation to work closely with their healthcare team to determine the most appropriate treatment option for their specific condition. The treatment plan will depend on the severity of the regurgitation, the presence of symptoms, and the individual’s overall health.