Necrotizing enterocolitis: causes, symptoms, diagnosis and treatment
Содержимое
Learn about the causes, symptoms, diagnosis, and treatment of necrotizing enterocolitis, a serious condition that affects the intestines of infants. Find out how this condition can be diagnosed, the common symptoms to look out for, and the available treatment options to manage this condition.
Necrotizing Enterocolitis (NEC) is a serious condition that affects the intestines of premature infants. It is characterized by inflammation and necrosis (death) of the bowel tissue, leading to a range of complications and potential long-term effects. NEC is a significant concern in neonatal care, as it is one of the leading causes of morbidity and mortality among premature infants.
The exact cause of NEC is not fully understood, but several risk factors have been identified. Premature birth, especially before 32 weeks of gestation, is a major risk factor for developing NEC. Other factors that increase the likelihood of NEC include a low birth weight, formula feeding instead of breast milk, a compromised immune system, and a history of intestinal problems.
There are several symptoms associated with NEC, and early recognition is crucial for prompt diagnosis and treatment. These symptoms may include feeding difficulties, abdominal distension, bloody stools, lethargy, temperature instability, and respiratory distress. It is important for healthcare providers to be vigilant in monitoring premature infants for these signs and symptoms, as timely intervention can significantly improve outcomes.
Diagnosing NEC involves a combination of clinical evaluation, laboratory tests, and imaging studies. A physical examination may reveal abdominal tenderness and swelling. Laboratory tests, such as blood tests and stool cultures, can help identify signs of infection or inflammation. Imaging studies, such as X-rays or ultrasounds, may be used to visualize any abnormalities in the intestine.
Treatment for NEC typically involves a multidisciplinary approach and may vary depending on the severity of the condition. In mild cases, treatment may involve the temporary cessation of oral feedings, intravenous fluids, and antibiotics. Severe cases may require surgery to remove the necrotic bowel tissue. Additionally, supportive care, such as respiratory support and close monitoring, is essential to manage complications and promote healing.
In conclusion, NEC is a serious condition that can have significant consequences for premature infants. Understanding the causes, recognizing the symptoms, and promptly diagnosing and treating NEC are essential for improving outcomes. Healthcare providers and parents alike should be educated about NEC to ensure early intervention and appropriate management of this potentially life-threatening condition.
Understanding Necrotizing Enterocolitis
Necrotizing enterocolitis (NEC) is a serious gastrointestinal disease that primarily affects premature infants. It is characterized by inflammation and damage to the intestines, which can lead to tissue death and perforation of the bowel. NEC is a medical emergency and requires immediate treatment.
The exact cause of NEC is unknown, but there are several risk factors that can increase a baby’s likelihood of developing the condition. These include premature birth, formula feeding, a weakened immune system, and a lack of blood flow to the intestines. While NEC can occur in full-term infants, it is most commonly seen in preemies.
Some of the symptoms of NEC include abdominal distension, bloody stools, feeding difficulties, and a decrease in bowel movements. It is important to seek medical attention if your baby displays any of these symptoms, as early diagnosis and treatment can improve the prognosis.
Diagnosing NEC typically involves a combination of physical exams, blood tests, and imaging studies. The doctor may perform a physical exam to check for signs of abdominal tenderness or a distended abdomen. Blood tests can help determine if there is an infection or inflammation present. Imaging studies, such as X-rays or ultrasounds, may be used to evaluate the condition of the intestines.
Treatment for NEC usually involves a combination of medical and surgical interventions. In mild cases, treatment may include antibiotics to fight infection, withholding oral feedings, and providing intravenous fluids. In more severe cases, surgery may be necessary to remove damaged portions of the intestine or to repair perforations.
Prevention is key when it comes to NEC. If your baby is at risk for NEC, there are steps you can take to reduce their chances of developing the condition. These include providing breast milk, practicing good hygiene, and avoiding overfeeding or underfeeding.
In conclusion, necrotizing enterocolitis is a serious and potentially life-threatening condition that affects premature infants. Understanding the causes, symptoms, and treatment options can help parents and healthcare providers recognize and address the condition in a timely manner.
Main Causes of Necrotizing Enterocolitis
Necrotizing enterocolitis (NEC) is a serious condition that primarily affects premature infants, especially those with low birth weight. While the exact cause of NEC is not fully understood, there are several factors that have been identified as potential causes or contributors to the development of this condition.
1. Premature birth: Premature infants, particularly those born before 32 weeks gestation, are at a higher risk of developing NEC. The immature digestive system of these babies is not fully developed, making them more susceptible to intestinal injury and infection.
2. Intestinal ischemia: Reduced blood flow to the intestines, known as intestinal ischemia, is considered a major contributing factor to the development of NEC. This can occur due to a variety of reasons, including low blood pressure, blood clotting disorders, and other conditions that restrict blood flow to the intestines.
3. Formula feeding: Infants who are fed with formula instead of breast milk are also at a higher risk of developing NEC. Breast milk contains essential nutrients and protective factors that help in the development and protection of the infant’s gastrointestinal tract. Formula feeding, on the other hand, may increase the risk of infection and inflammation in the intestines.
4. Bacterial colonization: The colonization of harmful bacteria in the intestines has been associated with the development of NEC. When the balance of bacteria in the gut is disrupted, it can lead to an overgrowth of harmful bacteria, which can cause inflammation and damage to the intestinal tissue.
5. Immature immune system: Premature infants have an immature immune system, which makes them more susceptible to infections and inflammatory conditions. This compromised immune system can contribute to the development of NEC.
6. Prenatal factors: Certain prenatal factors, such as maternal infections, placental abnormalities, and poor fetal growth, have also been linked to an increased risk of NEC. These factors can affect the development of the infant’s gastrointestinal tract and make them more vulnerable to the condition.
It is important to note that while these factors have been identified as potential causes of NEC, the exact mechanisms through which they contribute to the development of the disease are still being studied. Early recognition and management of these risk factors can help in reducing the incidence and severity of NEC in premature infants.
Common Symptoms of Necrotizing Enterocolitis
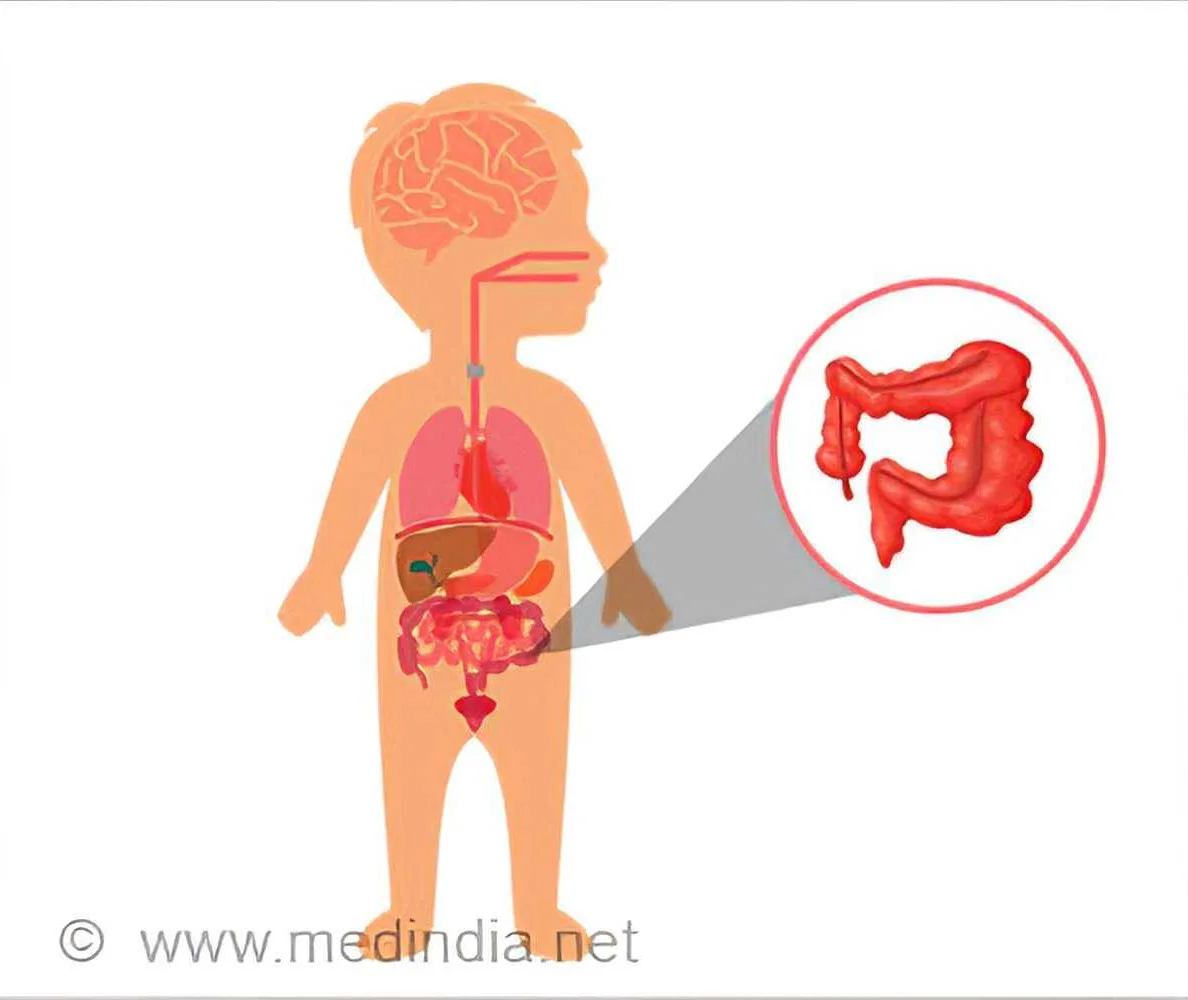
Necrotizing enterocolitis (NEC) is a serious condition that primarily affects premature infants. It is characterized by inflammation and necrosis (tissue death) in the intestines. Early recognition and diagnosis of NEC is important for timely treatment and improved outcomes.
The symptoms of NEC can vary depending on the severity of the condition. Common symptoms include:
- Abdominal distension: The baby’s abdomen may appear swollen or distended due to the accumulation of gas in the intestines.
- Bloody stools: The baby may pass stools that contain blood or have a bloody appearance.
- Feeding difficulties: Babies with NEC may have difficulty feeding, show signs of poor appetite, or refuse to eat altogether.
- Vomiting: NEC can cause frequent vomiting or forceful expulsion of stomach contents.
- Lethargy: Infants with NEC may seem unusually tired, lack energy, or have decreased activity levels.
- Temperature instability: NEC can cause fluctuations in body temperature, with the baby appearing excessively warm or cold.
- Respiratory difficulties: Some infants with NEC may experience breathing difficulties, including rapid breathing or labored breathing.
- Increased heart rate: The heart rate of a baby with NEC may be elevated, indicating a stress response.
- Apnea episodes: NEC can lead to periods of apnea, where the baby temporarily stops breathing.
If your baby exhibits any of these symptoms, it is important to seek immediate medical attention. Prompt diagnosis and treatment can help prevent complications and improve the chances of a successful recovery.
Diagnosing Necrotizing Enterocolitis
Diagnosing necrotizing enterocolitis (NEC) can be challenging, as it shares similar symptoms with other gastrointestinal conditions. However, there are several methods that doctors use to make an accurate diagnosis.
Firstly, the doctor will evaluate the baby’s medical history and conduct a physical examination. They will look for signs of abdominal distension, feeding problems, and a decreased stool output. These symptoms are common in NEC and can help raise suspicion.
Next, the doctor may order laboratory tests to assess the baby’s blood counts and inflammatory markers. Elevated white blood cell count and C-reactive protein levels may indicate an inflammatory process, suggesting NEC. Blood cultures may also be taken to rule out a bacterial infection.
In addition, imaging studies play a crucial role in diagnosing NEC. An abdominal X-ray can reveal signs of air in the bowel wall or pneumatosis intestinalis, which is one of the classic findings in NEC. Other findings, such as free air in the abdominal cavity or a dilated bowel, may indicate more severe disease.
If the doctor still has doubts or needs more detailed information, they may perform additional imaging tests, such as an abdominal ultrasound or a computed tomography (CT) scan. These tests can provide a more detailed view of the intestines and help confirm the diagnosis.
It is important to diagnose NEC promptly to prevent complications and provide appropriate treatment. If NEC is suspected, the baby may require close monitoring in the neonatal intensive care unit and consultations with pediatric surgeons or gastroenterologists to manage the condition effectively.