General information about the venous system
Содержимое
Learn about the venous system, which is responsible for carrying deoxygenated blood back to the heart. Understand its anatomy, function, and common conditions that can affect it. Explore the role of veins in maintaining a healthy circulatory system.
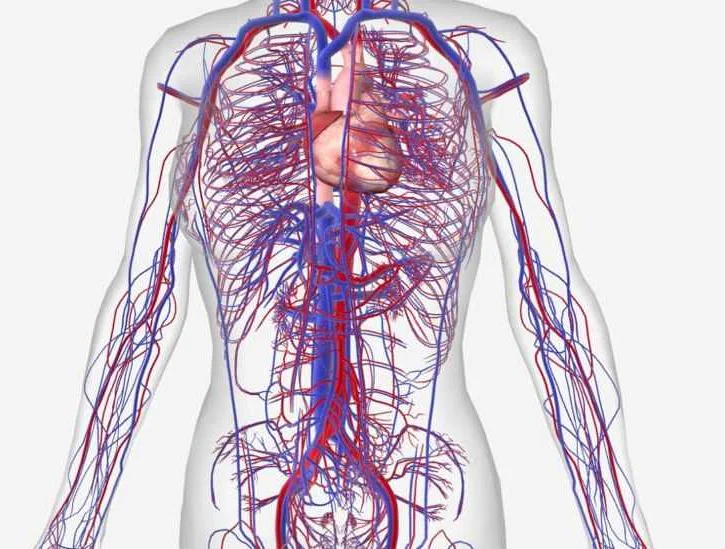
The venous system is a crucial component of the circulatory system, responsible for the return of deoxygenated blood back to the heart. It plays a vital role in maintaining the overall health and functioning of the body. Understanding the venous system is essential for healthcare professionals, as it can provide valuable insights into various medical conditions and help guide treatment decisions.
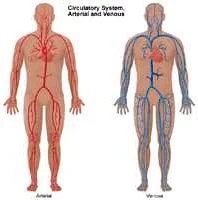
Comprised of a vast network of veins, the venous system carries blood from the capillaries to the heart. Unlike the arterial system, which transports oxygenated blood away from the heart, the venous system carries deoxygenated blood back to the heart, where it can be reoxygenated and recirculated. The veins are thinner and less muscular than arteries, relying on the contraction of surrounding skeletal muscles and valves within the veins themselves to promote blood flow.
One of the key features of the venous system is its ability to prevent the backward flow of blood, known as venous reflux. This is achieved through the presence of one-way valves within the veins, which ensure that blood flows in the correct direction towards the heart. However, dysfunction or damage to these valves can lead to conditions such as venous insufficiency or varicose veins, where blood pools and flows in the wrong direction. Understanding the structure and function of the venous system is crucial in diagnosing and treating such conditions.
In this comprehensive guide, we will explore the different components of the venous system, including the major veins and their branches, as well as the various conditions that can affect the venous system. We will delve into the anatomy and physiology of veins, discussing their structure, function, and role in overall cardiovascular health. Whether you are a healthcare professional looking to expand your knowledge or an individual seeking to understand more about the venous system, this guide will provide you with the essential information you need.
Understanding the Venous System and Its Functions
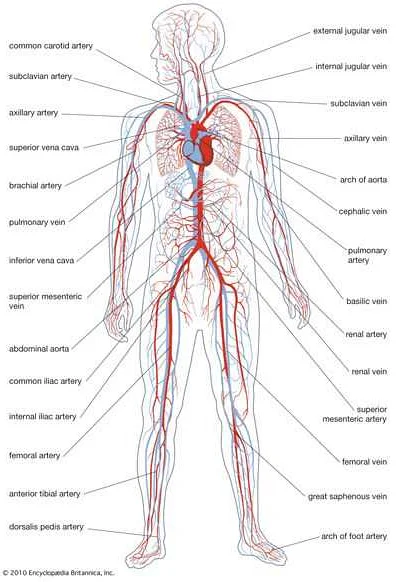
The venous system is a crucial component of the circulatory system, responsible for carrying deoxygenated blood back to the heart. While often overshadowed by the arterial system, the venous system plays a vital role in maintaining overall circulatory function.
One of the primary functions of the venous system is to transport blood from the capillaries, where oxygen and nutrients are delivered to tissues, back to the heart. This deoxygenated blood is then pumped to the lungs for oxygenation before being returned to the rest of the body via the arterial system.
The venous system also acts as a reservoir, capable of storing a significant portion of the body’s blood volume. This reservoir function allows for rapid adjustments in blood flow to meet the body’s changing needs. During periods of increased activity or stress, the veins constrict, shunting more blood to the arterial system, thereby ensuring that vital organs receive an adequate supply.
In addition to its transport and reservoir functions, the venous system plays a critical role in regulating blood pressure. Venous valves, located throughout the veins, help to prevent backflow and maintain the unidirectional flow of blood towards the heart. By preventing blood from pooling in the lower extremities, venous valves contribute to the maintenance of normal blood pressure levels.
Understanding the venous system and its functions is essential in diagnosing and managing various cardiovascular conditions. Disorders such as deep vein thrombosis, venous insufficiency, and varicose veins can impair the normal functioning of the venous system, leading to significant health complications if left untreated.
In conclusion, the venous system is a vital part of the circulatory system, responsible for transporting deoxygenated blood back to the heart. It serves as a reservoir and plays a role in regulating blood pressure. By understanding the functions of the venous system, healthcare professionals can better diagnose and treat cardiovascular conditions, ultimately improving patient outcomes.
Common Disorders and Diseases of the Venous System
The venous system plays a vital role in the circulation of blood throughout the body, and as such, it is susceptible to various disorders and diseases. Understanding these conditions is essential for both healthcare professionals and individuals seeking to maintain their vascular health. Here are some of the most common disorders and diseases of the venous system:
Varicose Veins: Varicose veins are enlarged, twisted veins that most commonly occur in the legs and feet. They are caused by weakened valves in the veins, which allow blood to flow backward and pool in the veins. Symptoms of varicose veins can include pain, swelling, and aching in the affected area. Treatment options range from lifestyle changes, such as exercise and wearing compression stockings, to more invasive procedures like sclerotherapy or vein stripping.
Deep Vein Thrombosis (DVT): Deep vein thrombosis occurs when a blood clot forms in one of the deep veins in the body, most commonly in the leg. Common risk factors for DVT include prolonged immobility, surgery, pregnancy, and certain medical conditions. Symptoms of DVT can include pain, swelling, warmth, and redness in the affected area. Treatment typically involves blood thinning medications to prevent the clot from growing or traveling to the lungs.
Chronic Venous Insufficiency (CVI): CVI is a condition in which the venous walls and valves in the legs are damaged, leading to poor blood flow back to the heart. This can result in symptoms such as leg swelling, pain, and skin changes like discoloration or ulcers. Treatment for CVI often involves lifestyle changes, such as exercise and elevation of the legs, as well as the use of compression stockings to improve blood flow.
Superficial Thrombophlebitis: Superficial thrombophlebitis is the inflammation of a superficial vein, usually in the legs. It is often caused by a blood clot forming in the vein due to injury or infection. Symptoms can include redness, warmth, and pain along the affected vein. Treatment typically involves anti-inflammatory medications, warm compresses, and the use of compression stockings.
Spider Veins: Spider veins are similar to varicose veins but are smaller and closer to the surface of the skin. They often appear as red or blue spiderweb-like patterns and are commonly found on the face and legs. While spider veins are generally harmless, some individuals may experience discomfort or self-consciousness. Treatment options include sclerotherapy, laser therapy, and vein stripping.
Phlebitis: Phlebitis is the inflammation of a vein, usually in the legs. It can be caused by trauma, infection, or an underlying medical condition. Symptoms can include pain, swelling, redness, and a firm, tender vein. Treatment for phlebitis usually involves rest, elevation of the affected limb, and the use of anti-inflammatory medications.
These are just a few examples of the common disorders and diseases that can affect the venous system. It is important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment options if you suspect any issues with your venous health.
Diagnostic Methods for Assessing Venous Health
Assessing venous health is crucial for diagnosing and managing venous disorders. There are several diagnostic methods available that help healthcare professionals evaluate the condition of the venous system.
Ultrasound: Ultrasound is the most commonly used diagnostic tool for assessing venous health. It uses sound waves to create images of the veins and measure blood flow. Doppler ultrasound, a specialized form of ultrasound, can provide detailed information about blood flow and detect any blockages or abnormalities.
CT Scan: Computed Tomography (CT) scan is another diagnostic method used to assess venous health. It uses x-rays and computer technology to create cross-sectional images of the veins. CT scan can help identify blood clots, tumors, or other abnormalities in the venous system.
Magnetic Resonance Imaging (MRI): MRI uses a strong magnetic field and radio waves to generate detailed images of the body. It can be used to assess venous health by providing information about blood flow, detecting abnormalities, and identifying the presence of blood clots.
Venography: Venography is an invasive diagnostic procedure that involves injecting a contrast dye into the veins and taking x-ray images. It provides detailed information about the venous system and can help identify blockages and other abnormalities.
Physical Examination: A physical examination by a healthcare professional can also provide valuable information about venous health. This may involve checking for visible varicose veins, swelling, or changes in skin color or texture.
Other Tests: In addition to these methods, there are other tests that can be used to assess venous health, such as blood tests to measure clotting factors or the presence of specific antibodies.
Overall, a combination of these diagnostic methods is often used to assess venous health and diagnose venous disorders accurately. It is essential to consult a healthcare professional for a proper evaluation and diagnosis.
Treatment Options for Venous Disorders
There are several treatment options available for venous disorders, depending on the severity and specific condition. These treatments aim to alleviate symptoms, improve blood flow, and prevent complications. Some of the common treatment options for venous disorders include:
- Compression therapy: This involves using compression stockings or bandages to apply pressure to the affected veins, improving blood flow and reducing swelling.
- Sclerotherapy: This is a minimally invasive procedure where a solution is injected into the affected veins, causing them to close off and eventually fade away.
- Laser therapy: This treatment uses laser energy to heat and destroy the affected veins, leading to their eventual disappearance.
- Vein stripping: In more severe cases, surgical removal of the affected veins may be necessary. This procedure is known as vein stripping and is usually reserved for large varicose veins.
- Endovenous techniques: These minimally invasive procedures involve the insertion of a catheter into the affected vein, which delivers heat or radiofrequency energy to close off the vein.
- Phlebectomy: This surgical procedure involves the removal of small varicose veins through tiny incisions. It is often performed in conjunction with other treatments.
It is important to note that the choice of treatment depends on various factors, including the type and severity of the venous disorder, as well as the patient’s overall health and preferences. Consulting with a qualified healthcare professional is essential to determine the most suitable treatment option for each individual case.