Top Treatment Options for Pancreatic Cancer
Содержимое
Learn about the best treatments available for pancreatic cancer, including surgery, chemotherapy, radiation therapy, immunotherapy, and targeted therapy. Find out about new research and clinical trials that offer hope for improved outcomes for patients with pancreatic cancer.
When it comes to pancreatic cancer, finding the right treatment plan is crucial for improving patient outcomes. With advancements in medical technology and research, there are now several effective treatment options available. In this comprehensive guide, we will explore the top treatments for pancreatic cancer and provide important information to help patients make informed decisions about their care.
One of the most common treatment approaches for pancreatic cancer is surgery. Surgery can be used to remove the tumor and surrounding tissue, and may be combined with other treatments such as chemotherapy or radiation therapy. It is important to note that not all patients with pancreatic cancer are eligible for surgery, as it depends on factors such as the stage and location of the tumor.
Chemotherapy is another commonly used treatment for pancreatic cancer. This treatment involves the use of drugs to kill cancer cells or stop them from dividing. Chemotherapy can be given before or after surgery, and may also be used to relieve symptoms and improve quality of life in advanced stages of the disease. It is typically administered through intravenous infusion, but can also be taken orally in some cases.
Radiation therapy, also known as radiotherapy, is often used in combination with surgery or chemotherapy to treat pancreatic cancer. This treatment uses high-energy particles or waves to destroy cancer cells. Radiation therapy can be given externally, where a machine directs radiation at the tumor, or internally, where radioactive materials are placed near the tumor. Like chemotherapy, radiation therapy can also be used to relieve symptoms and improve quality of life.
Understanding Pancreatic Cancer
Pancreatic cancer is a type of cancer that starts in the pancreas, a small organ located behind the stomach. The pancreas plays a crucial role in digestion and the production of hormones such as insulin.
Unfortunately, pancreatic cancer is often difficult to detect in its early stages, leading to a lower survival rate compared to other types of cancer. The symptoms of pancreatic cancer are vague and can be easily mistaken for other less serious conditions, making it challenging to diagnose.
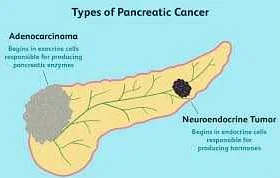
There are two main types of pancreatic cancer: exocrine pancreatic cancer and endocrine pancreatic cancer. Exocrine pancreatic cancer accounts for about 95% of all pancreatic cancer cases and starts in the cells that produce digestive enzymes. Endocrine pancreatic cancer, also known as pancreatic neuroendocrine tumors (PNETs), is less common and starts in the hormone-producing cells of the pancreas.
Risk factors for pancreatic cancer include smoking, age (most cases occur in people over 60), family history of pancreatic cancer, chronic pancreatitis, obesity, and certain genetic conditions.
Treatment options for pancreatic cancer depend on the stage of the disease and may include surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, and palliative care. A multidisciplinary approach involving a team of specialists is often necessary to develop an individualized treatment plan for each patient.
It is essential to raise awareness about pancreatic cancer and promote early detection through regular screenings, especially for individuals at high risk. Research and clinical trials are continuously advancing our understanding of pancreatic cancer and improving treatment options, giving hope to patients and their families.
Risk Factors and Prevention
Understanding the risk factors associated with pancreatic cancer can help individuals take proactive steps to reduce their risk and potentially prevent the development of this disease. While certain risk factors cannot be changed, such as age and family history, there are several modifiable risk factors that individuals can address.
Smoking: Tobacco use is one of the most significant risk factors for pancreatic cancer. It is estimated that smokers have a two to three times higher risk of developing pancreatic cancer compared to non-smokers. Quitting smoking can greatly reduce the risk of pancreatic cancer and improve overall health.
Obesity: Being overweight or obese can increase the risk of developing pancreatic cancer. Maintaining a healthy weight through exercise and a balanced diet can help reduce the risk of developing this disease.
Diabetes: Individuals with diabetes have a higher risk of developing pancreatic cancer. It is important for individuals with diabetes to manage their blood sugar levels and receive regular medical check-ups to monitor their pancreatic health.
Pancreatitis: Chronic inflammation of the pancreas, known as pancreatitis, can increase the risk of developing pancreatic cancer. Treating and managing pancreatitis can help reduce the risk of developing this disease.
Family History: Individuals with a family history of pancreatic cancer are at a higher risk of developing the disease. Regular screenings and genetic counseling may be recommended for individuals with a family history of pancreatic cancer.
Prevention: While not all cases of pancreatic cancer can be prevented, certain lifestyle changes can help reduce the risk of developing the disease. These include adopting a healthy diet rich in fruits and vegetables, limiting processed foods and red meat consumption, exercising regularly, quitting smoking, and moderating alcohol intake.
It is important for individuals to be aware of these risk factors and take appropriate steps to reduce their risk. Early detection and intervention can greatly improve the prognosis for individuals with pancreatic cancer.
Diagnosis and Staging
Diagnosing pancreatic cancer can be challenging due to its location deep within the abdomen. However, there are several diagnostic tests and imaging techniques that can help in the detection and evaluation of the disease.
The most common diagnostic tests for pancreatic cancer include:
| Imaging tests | These include computed tomography (CT) scans, magnetic resonance imaging (MRI), endoscopic ultrasound (EUS), and positron emission tomography (PET) scans. These tests can help identify the location and size of the tumor, as well as determine if it has spread to nearby organs or lymph nodes. |
| Blood tests | Specific blood tests, such as CA19-9 and CEA, can be used to detect certain substances in the blood that may indicate the presence of pancreatic cancer. However, these tests are not definitive and may produce false positives or negatives. |
| Biopsy | A biopsy involves removing a small sample of tissue from the pancreas to be examined under a microscope for cancer cells. This can be done through various techniques, including fine-needle aspiration, core biopsy, or surgical biopsy. |
Once pancreatic cancer has been diagnosed, staging is done to determine the extent and spread of the disease. The most commonly used staging system for pancreatic cancer is the TNM system, which stands for tumor, lymph nodes, and metastases.
The TNM system categorizes pancreatic cancer into four stages:
| Stage 0 | Also known as carcinoma in situ, the cancer is confined to the top layers of cells in the pancreas and has not spread. |
| Stage I | The cancer is limited to the pancreas and has not spread to nearby lymph nodes or other organs. |
| Stage II | The cancer has spread to nearby lymph nodes but has not spread to distant organs. |
| Stage III | The cancer has spread to nearby blood vessels or organs, such as the stomach, spleen, or bowel. |
| Stage IV | The cancer has spread to distant organs, such as the liver, lungs, or bones. |
Staging helps determine the appropriate treatment options and prognosis for pancreatic cancer patients. It allows doctors to plan the most effective course of action, whether it be surgery, radiation therapy, chemotherapy, or a combination of treatments.
Top Surgical Treatments
Whipple procedure
The Whipple procedure, also known as a pancreaticoduodenectomy, is a common surgical treatment for pancreatic cancer. It involves the removal of the head of the pancreas, the first part of the small intestine (duodenum), the gallbladder, and part of the bile duct. This procedure can be effective in removing tumors that are localized to the head of the pancreas.
Laparoscopic surgery
Laparoscopic surgery is a minimally invasive surgical approach that can be used to treat pancreatic cancer. This procedure involves making small incisions in the abdomen and using a camera and specialized surgical tools to remove tumors or parts of the pancreas. Laparoscopic surgery can be less invasive and have a faster recovery time compared to traditional open surgery.
Pancreatectomy
A pancreatectomy is a surgical procedure that involves the removal of all or part of the pancreas. This procedure can be used to treat pancreatic cancer by removing tumors and preventing their spread to other parts of the body. Depending on the location and stage of the cancer, a partial or total pancreatectomy may be performed.
Distal pancreatectomy
A distal pancreatectomy involves the removal of the tail and body of the pancreas. This surgical treatment is commonly used when the tumor is localized to the tail or body of the pancreas. It can be performed as an open surgery or laparoscopically, depending on the specific case.
Enucleation
Enucleation is a surgical procedure that involves the removal of tumors from the pancreas without removing any surrounding tissue. This treatment is often used for small, benign tumors or neuroendocrine tumors that are localized to one part of the pancreas. Enucleation can help preserve the function of the pancreas while removing the tumor.
Islet cell transplantation
Islet cell transplantation is a surgical treatment that involves the transplantation of insulin-producing cells from the pancreas into the liver. This procedure is primarily used for patients with chronic pancreatitis or severe diabetes. Islet cell transplantation can help improve insulin production and control blood sugar levels.
Palliative surgery
Palliative surgery is a surgical treatment that aims to alleviate symptoms and improve quality of life for patients with advanced pancreatic cancer. This can involve procedures such as biliary or gastric bypass to relieve jaundice and improve digestion. Palliative surgery is typically used when curative treatments are no longer an option.