Understanding Aortic Aneurysms and Dissections: An Overview
Содержимое
Learn about the causes, symptoms, diagnosis, and treatment options for aortic aneurysms and dissections, a potentially life-threatening condition that affects the body’s largest artery, the aorta. Gain an understanding of the risk factors, prevention strategies, and available surgical and non-surgical interventions for managing this serious cardiovascular condition.
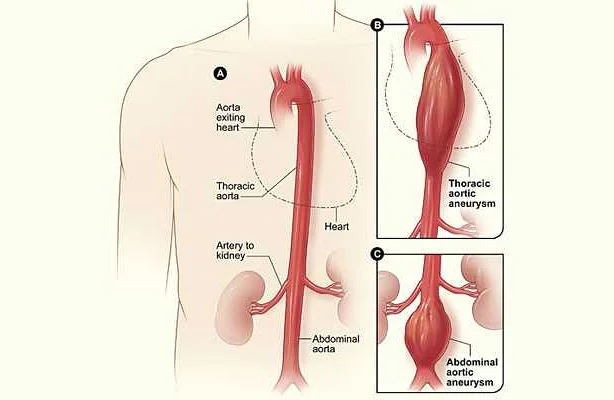
An aortic aneurysm is a condition that occurs when the aorta, the main blood vessel that carries oxygen-rich blood from the heart to the rest of the body, becomes weakened and bulges outwards. This bulging can cause the walls of the aorta to become thin and prone to rupture, which can be life-threatening.
Aortic aneurysms can occur in different parts of the aorta, including the ascending aorta, the aortic arch, and the descending aorta. They can be classified as either thoracic aortic aneurysms, which occur in the chest area, or abdominal aortic aneurysms, which occur in the abdomen.
Aortic dissection, on the other hand, is a condition that occurs when there is a tear in the inner layer of the aorta. This tear allows blood to flow between the layers of the aortic wall, causing them to separate. Aortic dissections can be life-threatening, as they can lead to decreased blood flow to vital organs or rupture of the aorta.
Understanding the risk factors and symptoms of aortic aneurysms and dissections is crucial for early detection and treatment. Risk factors for these conditions include age, family history, high blood pressure, smoking, and certain genetic disorders. Common symptoms may include chest or abdominal pain, shortness of breath, and a pulsating mass in the abdomen.
If you or a loved one is at risk for aortic aneurysms or dissections, it is important to seek medical attention promptly. Treatment options can vary depending on the size and location of the aneurysm or the severity of the dissection. Options may include medications to lower blood pressure, surgery to repair or replace the affected portion of the aorta, or endovascular repair, which involves inserting a stent or graft to reinforce the weakened area of the aorta.
Overall, aortic aneurysms and dissections are serious conditions that require prompt medical attention. By understanding the risks, symptoms, and treatment options, individuals can take proactive steps to protect their health and reduce the risk of life-threatening complications.
What are Aortic Aneurysms?
An aortic aneurysm refers to an abnormal bulging or ballooning of the aorta, which is the main blood vessel that carries oxygen-rich blood from the heart to the rest of the body. Aneurysms can develop in any section of the aorta, including the ascending aorta (the segment closest to the heart), the aortic arch (the curve in the aorta), or the descending aorta (the segment that extends down the chest and abdomen).
There are two main types of aortic aneurysms:
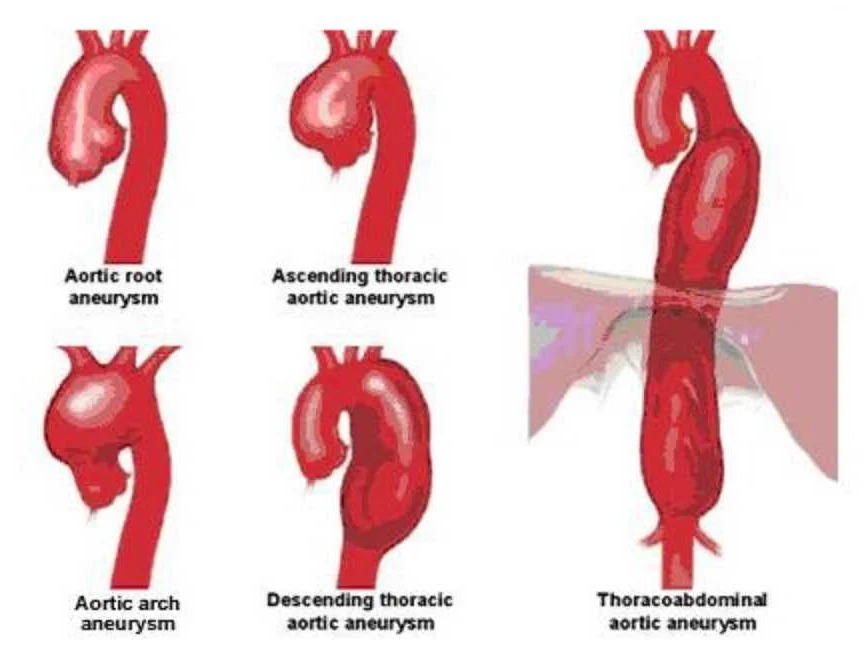
- Thoracic aortic aneurysms: These aneurysms occur in the part of the aorta that runs through the chest. They can be further classified as ascending aortic aneurysms, aortic arch aneurysms, or descending aortic aneurysms.
- Abdominal aortic aneurysms: These aneurysms develop in the lower part of the aorta, which extends through the abdomen. They are more common than thoracic aortic aneurysms.
Aortic aneurysms can be classified based on their size and shape:
- Saccular aneurysms: These aneurysms have a rounded shape and involve only a portion of the blood vessel wall.
- Fusiform aneurysms: These aneurysms have a more elongated shape and involve the entire circumference of the blood vessel wall.
Most aortic aneurysms are asymptomatic, meaning they do not cause any noticeable symptoms. However, they can progressively enlarge and weaken the aortic wall, which may lead to complications such as aortic dissection or rupture. Therefore, early detection and monitoring of aortic aneurysms are crucial for timely intervention and treatment.
Types of Aortic Aneurysms
Aortic aneurysms can be classified based on their location and shape. The main types of aortic aneurysms include:
| Abdominal Aortic Aneurysm (AAA) | An aneurysm that occurs in the abdominal portion of the aorta. It is the most common type of aortic aneurysm and often does not show any symptoms until it ruptures. |
| Thoracic Aortic Aneurysm (TAA) | An aneurysm that occurs in the thoracic portion of the aorta, which passes through the chest. This type of aneurysm can put pressure on nearby organs and structures, causing symptoms such as chest pain. |
| Thoracoabdominal Aortic Aneurysm | A combination of thoracic and abdominal aortic aneurysms, involving both the thoracic and abdominal portions of the aorta. This type of aneurysm is less common and may require complex surgery for treatment. |
| Fusiform Aortic Aneurysm | An aneurysm that bulges out on all sides of the blood vessel, resulting in a spindle-like shape. This type of aneurysm is usually associated with atherosclerosis, a buildup of plaque in the arteries. |
| Saccular Aortic Aneurysm | An aneurysm that bulges out on one side of the blood vessel, forming a sac-like structure. This type of aneurysm is often caused by an injury or infection and is less common than a fusiform aneurysm. |
It is important to diagnose and manage aortic aneurysms promptly, as they can lead to serious complications such as dissection or rupture. Treatment options include medication, lifestyle modifications, and surgical repair.
Causes and Risk Factors
An aortic aneurysm occurs when the wall of the aorta weakens and bulges outwards. There are several factors that can contribute to the development of an aortic aneurysm:
| Genetic factors | Age | Smoking |
| Inflammation | Gender | Hypertension |
| Infection | Race | Family history |
| Trauma | Connective tissue disorders |
Genetic factors can play a role in the development of an aortic aneurysm. People with a family history of the condition are more likely to develop one themselves.
Age is also a significant risk factor. Aortic aneurysms are more common in older individuals, particularly those over the age of 60.
Smoking is a major risk factor for the development of an aortic aneurysm. It weakens the walls of the blood vessels and increases the risk of aneurysm formation.
Gender can also play a role, with men being more likely to develop an aortic aneurysm compared to women.
Hypertension, or high blood pressure, is another risk factor. The increased pressure in the blood vessels can weaken the walls of the aorta over time.
Race can influence the risk of developing an aortic aneurysm. People of white and Hispanic descent are at a higher risk compared to those of African or Asian descent.
A history of connective tissue disorders such as Marfan syndrome or Ehlers-Danlos syndrome can make individuals more prone to developing aortic aneurysms.
Inflammation and infection can also weaken the walls of the aorta and contribute to the formation of an aneurysm.
Trauma, such as a car accident or injury, can cause the aorta to rupture or develop a tear, leading to an aortic dissection.
It is important to be aware of these causes and risk factors in order to take appropriate preventive measures and seek medical attention if necessary.
Symptoms and Diagnosis
Aortic aneurysms and dissections often do not cause symptoms until they become very large or rupture. However, when symptoms do occur, they can be severe and life-threatening. Some common symptoms of aortic aneurysms and dissections include:
- Chest or back pain: This is the most common symptom and is often described as a sudden, intense pain that may radiate to the neck, jaw, or arms.
- Trouble breathing or swallowing: As the aneurysm or dissection expands, it can put pressure on the airway or the esophagus, leading to difficulty breathing or swallowing.
- Hoarseness: Pressure on the recurrent laryngeal nerve can cause hoarseness or changes in the voice.
- Loss of consciousness: Aortic dissections can lead to decreased blood flow to the brain, resulting in fainting or loss of consciousness.
- Pulsatile mass: In some cases, a visible pulsating mass may be felt or seen in the abdomen or chest.
If a healthcare provider suspects an aortic aneurysm or dissection based on symptoms or physical examination findings, they will order further diagnostic tests to confirm the diagnosis. These tests may include:
- Computed tomography (CT) scan: This imaging test uses X-rays and a computer to create detailed images of the aorta and identify abnormalities.
- Magnetic resonance imaging (MRI): An MRI uses a powerful magnet and radio waves to produce detailed images of the aorta.
- Echocardiogram: This imaging test uses sound waves to create pictures of the heart and aorta.
- Angiography: A catheter is inserted into an artery and dye is injected to visualize the blood vessels and identify any abnormalities.
Early diagnosis of aortic aneurysms and dissections is crucial for effective treatment and to prevent life-threatening complications. Therefore, it is important to seek medical attention if you experience any symptoms that may indicate an aortic aneurysm or dissection.
Treatment Options
There are several treatment options available for aortic aneurysms and dissections. The choice of treatment depends on various factors such as the size and location of the aneurysm, the presence of symptoms, and the overall health of the patient. The main treatment options include:
1. Medical Management: This involves closely monitoring the aneurysm or dissection with regular imaging tests and managing risk factors such as high blood pressure and smoking. Medications may be prescribed to control blood pressure and reduce the risk of rupture or further growth of the aneurysm.
2. Endovascular Repair: This minimally invasive procedure involves inserting a stent graft into the aorta to reinforce the weakened or damaged wall of the aneurysm or dissection. The stent graft acts as a scaffolding to redirect blood flow, relieving pressure on the weakened area and reducing the risk of rupture.
3. Open Surgical Repair: In some cases, open surgery may be necessary to repair the aortic aneurysm or dissection. This procedure involves removing the damaged portion of the aorta and replacing it with a synthetic graft. Open surgical repair is usually reserved for complex cases or when endovascular repair is not feasible.
4. Hybrid Procedures: These procedures combine elements of both endovascular repair and open surgical repair. They may be performed in cases where the anatomy of the aneurysm or dissection is not suitable for either technique alone, or when there are unique patient factors that require a customized approach.
5. Watchful Waiting: In some cases, particularly when the aneurysm is small and not causing symptoms, a strategy of watchful waiting may be adopted. This involves regular monitoring of the aneurysm with imaging tests to ensure it is not growing or causing any complications. Surgery or other interventions may be considered if the aneurysm reaches a certain size or shows signs of enlargement or vulnerability.
It is important to consult with a healthcare provider to determine the most appropriate treatment option for an individual case.