Ventricular fibrillation
Содержимое
Ventricular fibrillation is a life-threatening arrhythmia that occurs when the heart’s electrical system malfunctions, causing the lower chambers of the heart to quiver instead of pumping blood effectively. This article provides an overview of ventricular fibrillation, including its causes, symptoms, diagnosis, and treatment options.
Ventricular fibrillation is a life-threatening cardiac arrhythmia that occurs when the heart’s ventricles contract in a rapid and disorganized manner. This condition disrupts the heart’s normal electrical signals, leading to an ineffective pumping of blood throughout the body. If left untreated, ventricular fibrillation can rapidly progress to cardiac arrest and cause death within minutes.
There are several underlying causes that can trigger ventricular fibrillation. One common cause is coronary artery disease, which occurs when the arteries that supply blood to the heart become narrowed or blocked. Other causes include heart attacks, electrolyte imbalances, drug overdose, and certain genetic conditions. Additionally, previous heart surgeries or structural abnormalities of the heart can also increase the risk of ventricular fibrillation.
The symptoms of ventricular fibrillation can be sudden and severe. They may include a loss of consciousness, no pulse, and absence of breathing. In some cases, individuals may experience chest pain, dizziness, or palpitations before the onset of ventricular fibrillation. It is important to note that ventricular fibrillation requires immediate medical attention, as every minute without treatment reduces the chances of survival.
Treatment for ventricular fibrillation involves the use of an automated external defibrillator (AED) to deliver an electric shock to the heart. This shock aims to restore a normal heartbeat by depolarizing the cardiac cells. In addition to defibrillation, cardiopulmonary resuscitation (CPR) is typically performed to maintain blood flow until more advanced medical care can be provided. After successful resuscitation, further treatment options may include medications, implantable cardioverter-defibrillators (ICDs), or ablation procedures to prevent future episodes of ventricular fibrillation.
In conclusion, ventricular fibrillation is a serious cardiac condition that requires immediate medical intervention. Understanding the causes, recognizing the symptoms, and knowing the appropriate treatment options can help save lives. If you or someone you know experiences symptoms of ventricular fibrillation, don’t hesitate to seek emergency medical assistance.
Understanding Ventricular Fibrillation
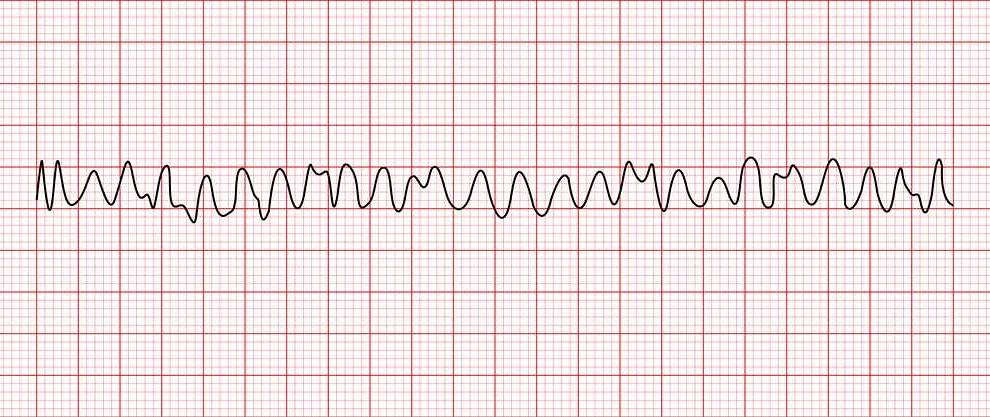
Ventricular fibrillation is a serious cardiac condition that can be life-threatening if not promptly treated. It occurs when the heart’s electrical signals become chaotic, causing the ventricles (the lower chambers of the heart) to quiver instead of contracting normally. This erratic electrical activity prevents the heart from effectively pumping blood to the rest of the body, leading to a sudden loss of consciousness and, if left untreated, death.
Ventricular fibrillation is typically the result of underlying heart conditions, such as coronary artery disease, heart attack, or cardiomyopathy. Other factors, such as certain medications, electrolyte imbalances, or genetic abnormalities, can also contribute to the development of ventricular fibrillation.
Recognizing the symptoms of ventricular fibrillation is crucial for prompt medical intervention. Common symptoms include sudden loss of consciousness, no pulse, and abnormal breathing. In some cases, individuals may experience chest pain, shortness of breath, or palpitations before the onset of ventricular fibrillation.
Treating ventricular fibrillation involves immediate cardiopulmonary resuscitation (CPR) and the use of an automated external defibrillator (AED) to restore a normal heart rhythm. If necessary, medications or invasive procedures, such as electrical cardioversion or implantable cardioverter-defibrillator (ICD) placement, may be utilized to prevent future episodes of ventricular fibrillation.
Prevention of ventricular fibrillation focuses on managing underlying heart conditions, such as hypertension, diabetes, and high cholesterol, through lifestyle modifications and appropriate medication. It’s also important to avoid triggers, such as excessive alcohol consumption or illicit drug use, that can increase the risk of ventricular fibrillation.
In conclusion, understanding ventricular fibrillation is essential for individuals to recognize the symptoms, seek immediate medical assistance, and receive appropriate treatment. By taking preventive measures and addressing underlying heart conditions, individuals can reduce their risk of developing ventricular fibrillation and its potentially fatal consequences.
Causes of Ventricular Fibrillation
Ventricular fibrillation is a life-threatening condition that occurs when the heart’s electrical signals become chaotic, causing the lower chambers of the heart (ventricles) to quiver or “fibrillate” instead of pumping blood effectively. Several factors can trigger ventricular fibrillation, including:
- Coronary artery disease: The most common cause of ventricular fibrillation is a blockage in the coronary arteries that supply blood to the heart muscle. When the blood flow to the heart is restricted, it can lead to the development of abnormal electrical signals and ultimately result in ventricular fibrillation.
- Heart attack: A heart attack occurs when a coronary artery becomes completely blocked, depriving the heart muscle of oxygen. This lack of oxygen can disrupt the heart’s electrical system and trigger ventricular fibrillation.
- Heart disease: Various forms of heart disease, such as cardiomyopathy (weakening of the heart muscle) and heart valve problems, can make the heart more susceptible to ventricular fibrillation. These conditions may disrupt the heart’s normal electrical signals and lead to fibrillation.
- Electrolyte imbalances: Abnormal levels of electrolytes, such as potassium, sodium, and calcium, can interfere with the heart’s electrical activity. This can increase the risk of ventricular fibrillation.
- Drug use: Certain drugs, such as cocaine and amphetamines, can stimulate the heart and disrupt its normal electrical signals. This can potentially lead to ventricular fibrillation.
- Electric shock: A severe electrical shock, such as those encountered in electrical accidents or lightning strikes, can disrupt the heart’s electrical system and cause ventricular fibrillation.
- Inherited conditions: In some cases, ventricular fibrillation may be caused by inherited conditions that affect the heart’s electrical system. These conditions, such as long QT syndrome or Brugada syndrome, can make individuals more prone to abnormal heart rhythms, including ventricular fibrillation.
It’s important to identify and address the underlying causes of ventricular fibrillation to prevent its occurrence and reduce the risk of life-threatening complications. If you experience symptoms of ventricular fibrillation, it’s crucial to seek immediate medical attention for proper diagnosis and treatment.
Risk Factors for Ventricular Fibrillation
Ventricular fibrillation is a life-threatening cardiac arrhythmia that can cause sudden cardiac arrest. While the exact cause of ventricular fibrillation is often unknown, there are several risk factors that can increase a person’s likelihood of experiencing this dangerous condition.
1. Coronary artery disease: The most common risk factor for ventricular fibrillation is coronary artery disease, which occurs when the arteries that supply blood to the heart become narrowed or blocked. This can lead to a heart attack and increase the risk of ventricular fibrillation.
2. Previous heart attack: Individuals who have previously had a heart attack are at a higher risk of developing ventricular fibrillation. Scar tissue from a heart attack can disrupt the electrical signals in the heart, leading to abnormal rhythms.
3. Heart failure: Heart failure, a condition in which the heart is unable to pump enough blood to meet the body’s needs, can also increase the risk of ventricular fibrillation. The weakened heart muscles can lead to irregular electrical activity and trigger an episode of ventricular fibrillation.
4. Cardiomyopathy: Certain types of cardiomyopathy, such as hypertrophic cardiomyopathy and dilated cardiomyopathy, can predispose individuals to ventricular fibrillation. These conditions affect the structure and function of the heart, making it more susceptible to abnormal rhythms.
5. Family history: A family history of sudden cardiac death or ventricular fibrillation can increase an individual’s susceptibility to the condition. Genetic factors may play a role in the development of abnormal electrical activity in the heart.
6. Use of certain medications: Certain medications, such as antiarrhythmic drugs, can potentially increase the risk of ventricular fibrillation. It is important to discuss the potential risks and benefits of these medications with a healthcare provider.
7. Illicit drug use: Illicit drug use, particularly the use of stimulants like cocaine and amphetamines, can increase the risk of ventricular fibrillation. These drugs can disrupt the normal electrical activity of the heart and increase the likelihood of arrhythmias.
8. Electrolyte imbalances: Imbalances in electrolytes, such as potassium and magnesium, can disrupt the electrical signals in the heart and lead to ventricular fibrillation. It is important to maintain a healthy balance of electrolytes through proper nutrition and hydration.
While these risk factors can increase the likelihood of developing ventricular fibrillation, it is important to note that the condition can occur in individuals without any identifiable risk factors. It is essential to seek immediate medical attention if experiencing symptoms of ventricular fibrillation, such as chest pain, shortness of breath, and loss of consciousness.