Ventricular tachycardia
Содержимое
Learn about ventricular tachycardia, a rapid heartbeat originating in the ventricles of the heart. Understand the causes, symptoms, and treatment options for this condition.
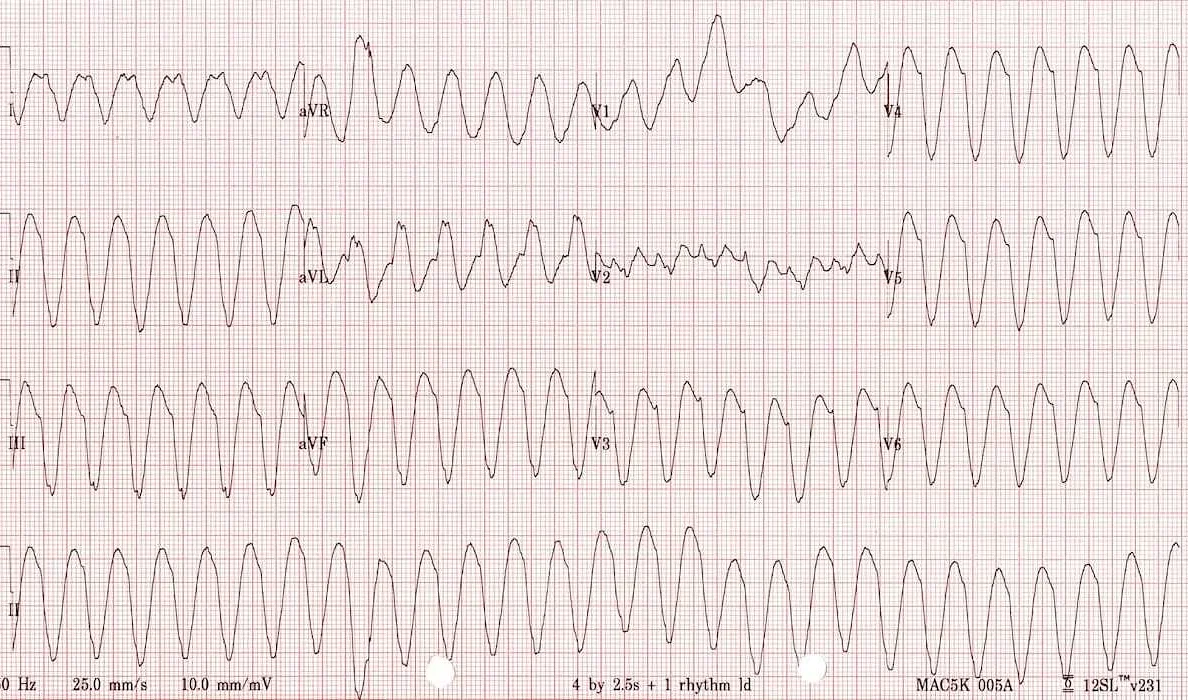
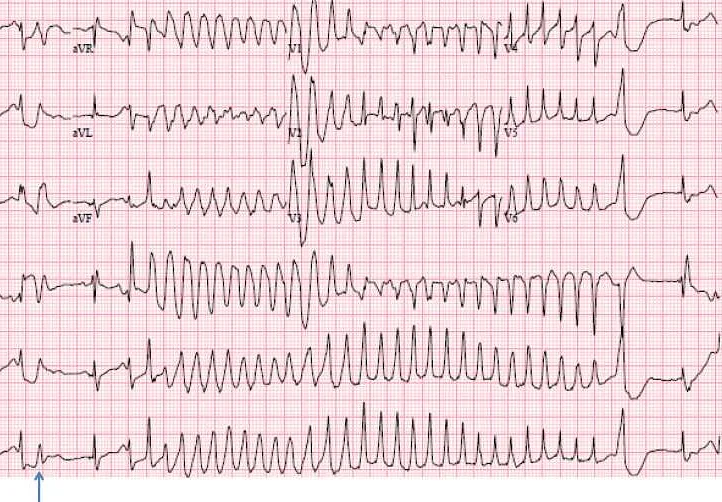
Ventricular tachycardia is a cardiac rhythm disorder characterized by a rapid heart rate originating from the ventricles, the lower chambers of the heart. This condition can be potentially life-threatening and requires prompt medical attention. Ventricular tachycardia can occur in individuals with or without underlying heart disease, and it can present with various symptoms ranging from mild to severe.
The causes of ventricular tachycardia can be diverse. They may include structural heart abnormalities, such as heart attacks, cardiomyopathy, or heart defects present at birth. Other factors that can contribute to the development of ventricular tachycardia include electrolyte imbalances, certain medications, and illegal drugs. In some cases, the exact cause may remain unknown.
Individuals experiencing ventricular tachycardia may exhibit symptoms such as palpitations, dizziness, shortness of breath, chest pain, or fainting. However, some individuals with ventricular tachycardia may not experience any symptoms, and the condition may only be detected during a routine medical examination or an electrocardiogram (ECG).
Treatment options for ventricular tachycardia depend on the underlying cause, the severity of symptoms, and other individual factors. In some cases, no treatment may be needed if the condition is well-tolerated and does not pose a substantial risk. However, for individuals with severe symptoms or a high risk of complications, treatment may involve medications to control heart rate and prevent abnormal heart rhythms, as well as procedures like catheter ablation or implantation of an implantable cardioverter-defibrillator (ICD).
Causes of Ventricular Tachycardia
Ventricular tachycardia is a condition characterized by a rapid heart rhythm originating in the ventricles, the lower chambers of the heart. There are several factors that can cause ventricular tachycardia, including:
- Coronary artery disease: The most common cause of ventricular tachycardia is coronary artery disease, which occurs when the arteries that supply blood to the heart become narrowed or blocked.
- Heart attack: Ventricular tachycardia can also occur after a heart attack, when the damaged heart tissue disrupts the normal electrical signals in the heart.
- Cardiomyopathy: Certain types of cardiomyopathy, such as dilated cardiomyopathy or hypertrophic cardiomyopathy, can increase the risk of ventricular tachycardia.
- Heart valve problems: Conditions like mitral valve prolapse, mitral regurgitation, or aortic stenosis can disrupt the normal functioning of the heart and lead to ventricular tachycardia.
- Electrolyte imbalances: Abnormal levels of potassium, calcium, or magnesium in the blood can interfere with the heart’s electrical system and contribute to the development of ventricular tachycardia.
- Drug side effects: Certain medications, such as antiarrhythmics, antipsychotics, or stimulants, can increase the risk of ventricular tachycardia as a side effect.
- Genetic factors: In some cases, ventricular tachycardia may be inherited due to genetic abnormalities that affect the heart’s electrical system.
It’s important to identify the underlying cause of ventricular tachycardia in order to determine the most appropriate treatment plan. If you experience symptoms of ventricular tachycardia, it is essential to seek medical attention to receive a proper diagnosis and create an individualized treatment approach.
Heart Disease and Damage
Heart disease can be a leading cause of ventricular tachycardia. Conditions such as coronary artery disease, heart attack, and heart failure can all contribute to the development of ventricular tachycardia.
Coronary artery disease occurs when the blood vessels that supply the heart with oxygen-rich blood become narrowed or blocked. This can lead to a heart attack, where a section of the heart muscle is damaged due to a lack of blood flow. Heart attacks can cause scar tissue to form in the heart, which can disrupt the normal electrical pathways and lead to ventricular tachycardia.
Heart failure is a condition in which the heart is unable to pump enough blood to meet the body’s needs. This can be caused by underlying heart disease, high blood pressure, or other factors. When the heart is not functioning properly, it can lead to abnormal heart rhythms, including ventricular tachycardia.
In addition to these conditions, other factors such as congenital heart defects, heart valve problems, and certain medications can also increase the risk of ventricular tachycardia.
If you have been diagnosed with a heart condition or have a history of heart disease, it is important to work closely with your healthcare provider to manage your condition and reduce your risk of complications, including ventricular tachycardia.
Disclaimer: This information is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Electrolyte Imbalance
Ventricular tachycardia can be caused or exacerbated by electrolyte imbalances in the body. Electrolytes are minerals that carry an electric charge and are crucial for the proper functioning of the body’s cells and organs, including the heart.
An imbalance in electrolyte levels can disrupt the electrical signals that regulate the heart’s rhythm, leading to the development of ventricular tachycardia. Common electrolytes that play a role in heart function include potassium, sodium, calcium, and magnesium.
Low levels of potassium, known as hypokalemia, can increase the risk of ventricular tachycardia. Potassium helps regulate the electrical signals in the heart and a deficiency can lead to abnormal heart rhythms. Similarly, imbalances in sodium, calcium, and magnesium levels can also contribute to the development of ventricular tachycardia.
Electrolyte imbalances can occur due to various factors, including certain medications, excessive sweating, vomiting, diarrhea, kidney problems, and hormonal imbalances. Additionally, individuals with certain medical conditions, such as heart failure or kidney disease, may be more susceptible to electrolyte imbalances.
If an electrolyte imbalance is suspected to be the cause of ventricular tachycardia, medical professionals may perform blood tests to assess the levels of key electrolytes in the body. Treatment may involve addressing the underlying cause of the imbalance, such as adjusting medications or treating the underlying medical condition.
In some cases, supplementation or intravenous administration of specific electrolytes may be necessary to restore balance and stabilize the heart’s rhythm. It is important to work closely with a healthcare provider to monitor and manage electrolyte imbalances to reduce the risk of ventricular tachycardia and other potential complications.
Medications and Drugs
Ventricular tachycardia is a serious condition that requires immediate medical attention. There are several medications and drugs that can be used to treat ventricular tachycardia and manage its symptoms. These medications and drugs work by slowing down the heart rate and restoring normal rhythm.
One commonly prescribed medication for ventricular tachycardia is antiarrhythmic drugs. These drugs help to control abnormal heart rhythms by blocking the electrical signals that cause them. Some commonly prescribed antiarrhythmic drugs include amiodarone, lidocaine, and procainamide.
In addition to antiarrhythmic drugs, calcium channel blockers may also be used to treat ventricular tachycardia. These medications work by relaxing the blood vessels and reducing the workload on the heart. Some commonly prescribed calcium channel blockers include diltiazem and verapamil.
Another class of medications that can be used to treat ventricular tachycardia is beta blockers. Beta blockers work by blocking the effects of adrenaline on the heart, thereby slowing down the heart rate and reducing the workload. Some commonly prescribed beta blockers include metoprolol and propranolol.
In severe cases of ventricular tachycardia, doctors may prescribe anti-arrhythmic medications that are administered intravenously in a hospital setting. These medications are used to quickly control the abnormal heart rhythm and restore normal heart function.
It is important to note that the use of medications and drugs to treat ventricular tachycardia should always be done under the supervision of a qualified healthcare professional. They will determine the appropriate medication and dosage based on the individual patient’s condition and medical history.
| Amiodarone | Yes |
| Lidocaine | Yes |
| Procainamide | Yes |
| Diltiazem | Yes |
| Verapamil | Yes |
| Metoprolol | Yes |
| Propranolol | Yes |
Symptoms of Ventricular Tachycardia
Ventricular tachycardia is a condition characterized by a fast and irregular heartbeat that originates in the lower chambers of the heart, called the ventricles. This abnormal heart rhythm can lead to a decrease in blood flow to the body and can be a life-threatening condition.
The symptoms of ventricular tachycardia can vary from person to person. Some individuals may not experience any symptoms, while others may have noticeable signs. The most common symptoms of ventricular tachycardia include:
- Rapid heartbeat: People with ventricular tachycardia often experience a heartbeat that is faster than normal. The heart rate during an episode of ventricular tachycardia is usually above 100 beats per minute.
- Palpitations: Palpitations are a sensation in the chest that feels like a pounding or racing heart. This symptom is commonly reported by individuals with ventricular tachycardia.
- Dizziness: Feeling lightheaded or dizzy is another common symptom of ventricular tachycardia. This can occur due to decreased blood flow to the brain during episodes of rapid heart rate.
- Chest discomfort: Some individuals may experience chest discomfort or pain during episodes of ventricular tachycardia. This can range from a mild pressure or tightness sensation to severe chest pain.
- Fainting: In severe cases, ventricular tachycardia can cause a sudden loss of consciousness or fainting. This occurs when the heart is unable to pump enough blood to the brain.
- Shortness of breath: Rapid and irregular heartbeats can affect the heart’s ability to pump blood efficiently, leading to shortness of breath during physical activity or at rest.
If you experience any of these symptoms, especially if they are persistent or severe, it is important to seek medical attention. Ventricular tachycardia can be a serious condition that requires prompt diagnosis and treatment to prevent complications.